- 31 March 2020
- 7 min read
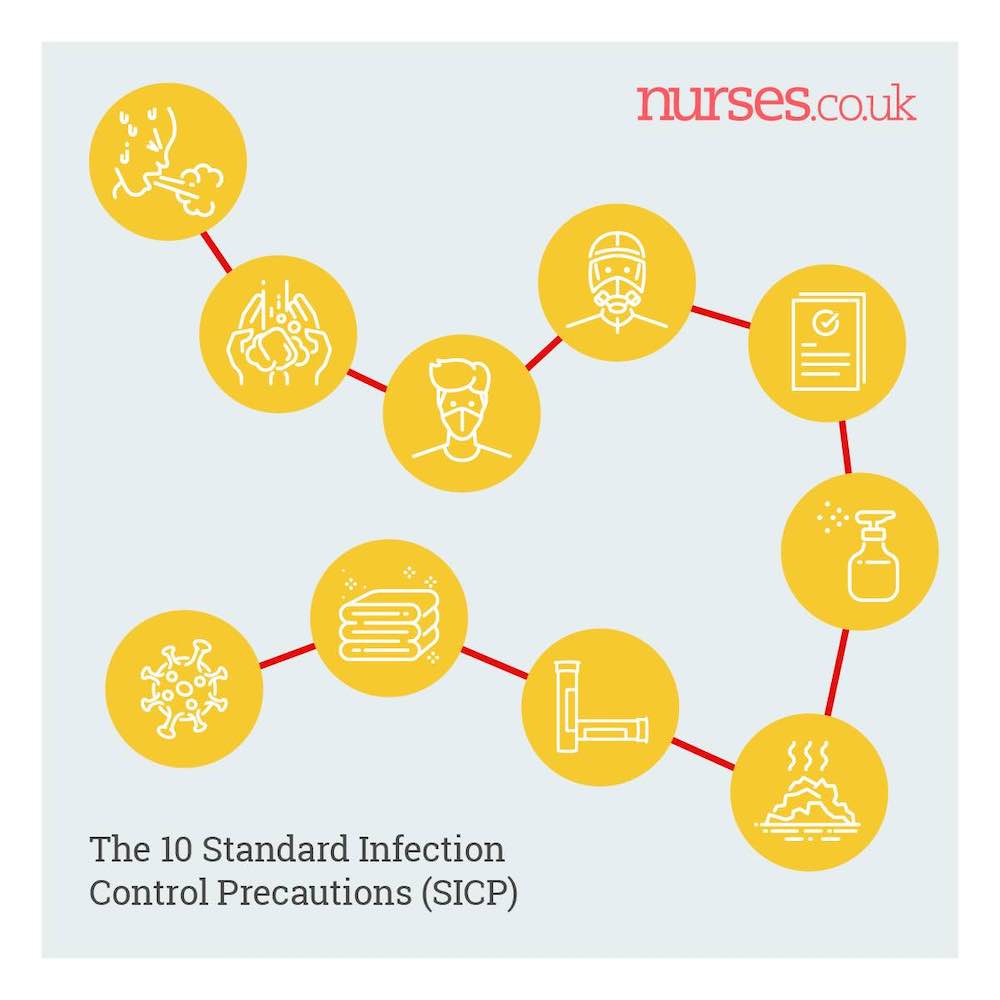
Your guide to the 10 Standard Infection Control Precautions (SICPs)
Subscribe "You can promote respiratory and cough hygiene with your patients too. Providing tissues, plastic bags for used tissues and hand washing stations will all help."
"You can promote respiratory and cough hygiene with your patients too. Providing tissues, plastic bags for used tissues and hand washing stations will all help."In view of the Coronavirus crisis here's a reminder of the 10 Standard Infection Control Precautions.
Topics covered in this article
The 10 Standard Infection Control Precautions (SICP)
1. Patient assessment for infection risk
3. Respiratory and cough hygiene
4. Personal protective equipment (PPE)
5. Safe management of equipment
6. Safe management of environment
7. Safe management of blood and body fluids
9. Safe disposal of waste (including sharps)
10. Occupational safety & Exposure
Thank you Josie!
Josie Winter of Advanced Clinical Solutions helped put this article together. You can find Josie and her team - if you need help dealing with compliance audits, clinical training, safety investigations, supervision/coaching of staff - get in touch with Josie!







About this contributor
Clinical Consultant
I’ve worked for the NHS - originally as an ODP - and for private healthcare organisations including a large corporate med-tech organisation. I’ve developed and delivered hundreds of clinical audits and quality improvement plans and trained thousands of healthcare staff in various clinical skills. I co-founded and head up a consultancy that helps healthcare providers achieve enhanced patient safety.
More by this contributorWant to get involved in the discussion?
Log In Subscribe to comment